News &
Insights
24 April 2024
Core Digital Measures of Sleep
Access to real world sleep assessment technology has undergone a dramatic expansion, revolutionising the landscape […]
Share This Post, Choose Your Platform!

Access to real world sleep assessment technology has undergone a dramatic expansion, revolutionising the landscape for sleep researchers. Collaborating closely with DATAcc, an FDA collaborative community hosted by DiMe, we’ve been at the forefront of standardising parameters of sleep measurement, streamlining the growing complexity that sleep researchers are facing.
Through collective insights from us and our industry colleagues, DATAcc has crafted a framework: Core Digital Measures of Sleep. This framework, alongside accompanying resources, aims to bolster the adoption of human-centric digital measures across the field.
Sleep plays a crucial role in various aspects of health and is linked to numerous conditions. Better sleep generally indicates better health, while disrupted sleep can indicate or cause chronic conditions. Measuring sleep disturbance facilitates the development of improved interventions and treatment options.
Challenging Contemporary Sleep Research Measurement Methods
The current landscape of sleep measurement in research and clinical care is being challenged by new methods. These digital approaches are less cumbersome and intrusive and give access to new insights in the natural sleep environment over long periods without compromising measurement accuracy.
Home-based sleep monitoring, exemplified by technologies like the GENEActiv wearable, heralds a transformative shift. Wearable technology not only minimises patient burden but also allows participants to be evaluated in their environment, devoid of additional stressors. Moreover, they enable long-term evaluation and yield more comprehensive real world data, laying the groundwork for personalised interventions tailored to individual needs and fostering a more holistic understanding of sleep patterns.
At the heart of this evolution lies the establishment of a set of core digital measures, essential for ensuring the validity and consistency of data collection. In this endeavour, DATAcc, hosted by DiMe, are spearheading improved methodologies and facilitating the seamless remote collection of sleep data—all from the comfort and familiarity of a patient’s own home and bed.
Importance of Sleep Digital Measures
Activinsights has a diverse catalogue of over 150 digital measures at our disposal of which sleep digital measures are a significant part and can greatly enhance the depth of insight into any study. Digital measures of sleep form the foundational elements for potential clinical trial endpoints and significant digital health biomarkers
DiMe defines the Core Digital Measures of Sleep framework as standardised benchmarks with mature measurement solutions used across the industry to measure sleep, making it easier to compare data. This standardisation not only enhances efficiency but also amplifies the efficacy of digital clinical measures. With this optimised set of core digital clinical measures in sleep, health professionals can increase the availability of high-quality, standardised, and transparent sleep research in the naturalistic environment across therapeutic areas. This transformation holds the promise of advancing population health and addressing myriad diseases.
Employing the core set of sleep measures will not only bolster transparency in research methodologies but also support consistency across projects– reducing risk, accelerating projects, and helping communication with regulators.
Why are we supporting DiMe’s initiative?
We are backing DiMe’s DATAcc initiative for several compelling reasons that resonate deeply with our mission and expertise.
Drawing on our extensive experience in the sleep research domain, we recognise the paramount importance of standardisation. DiMe’s efforts align with our advocacy for industry-wide standardisation. This initiative represents a significant step towards establishing uniformity in sleep research methodologies—a cause we’ve championed for years.
One of the ways we have been aiming for standardisation is by designing our wearable, the GENEActiv, to output unfiltered, sensor-level data to enable seamless transitions from traditional actigraphy devices, to our modern technologies. The integration of historical data prevents data loss and prioritises the continuation of long-term studies. Our commitment to inter-device compatibility is inspired by our advocacy for establishing greater uniformity in all research methodologies including sleep.
Furthermore, DiMe’s initiative serves as a vital resource for researchers bringing real world sleep measures into their studies for the first time. It provides a foundational framework, offering a clear starting point for those navigating the complexities of sleep measurement. For seasoned researchers, these guidelines formalise and streamline practices that they may have informally adopted, potentially requiring only minor adjustments for alignment.
In essence, our support for DiMe’s initiative reflects our commitment to advancing the field of sleep research through standardisation, compatibility, and accessibility, ultimately fostering innovation and progress in understanding sleep and its implications for health and well-being.
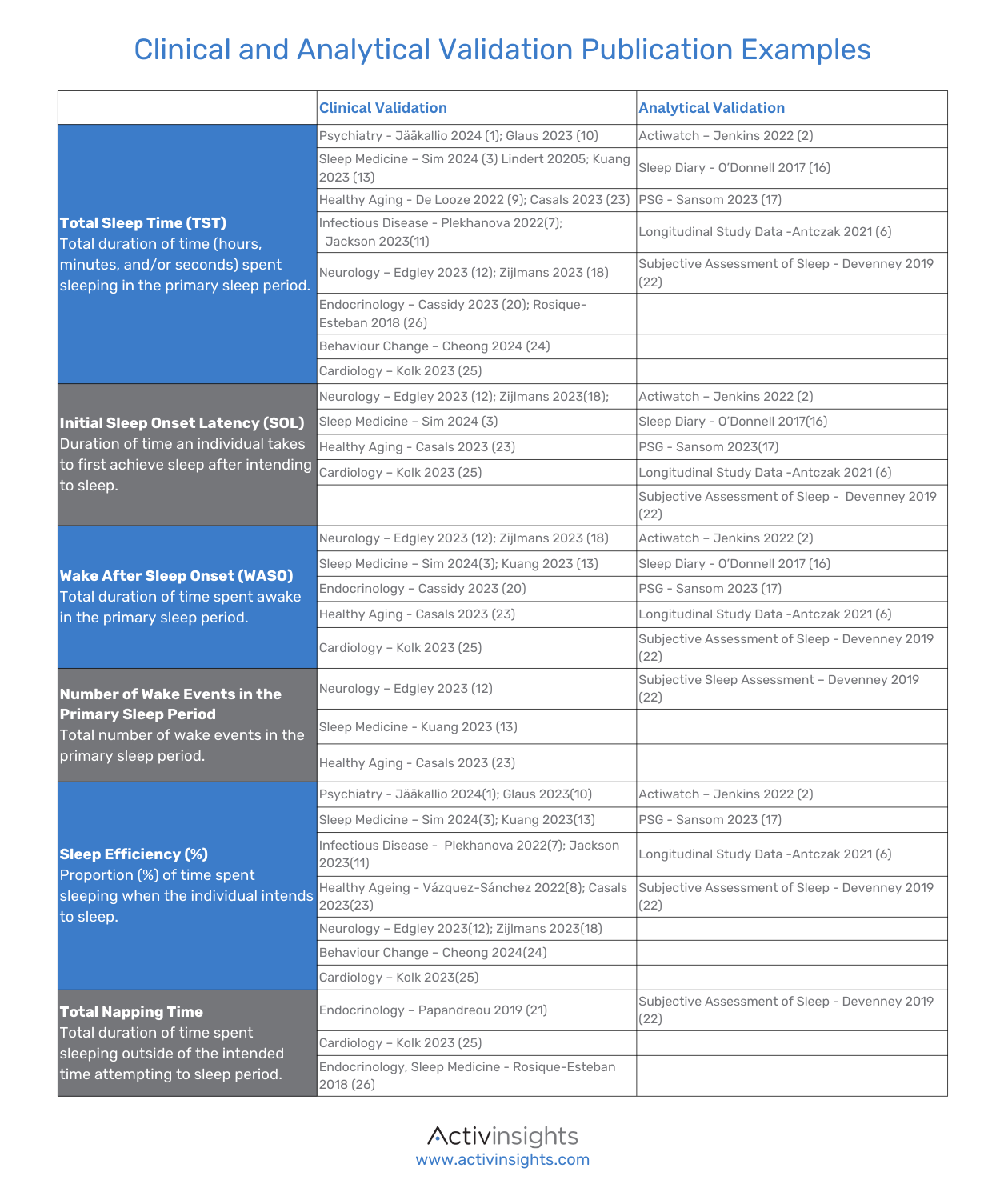
Validation
We are proud to affirm that our technologies stand on a solid foundation, with over 1100 publications attesting to their widespread use, efficacy and reliability. Moreover, they have been deployed in over 200 clinical trials, further cementing their reputation as a trusted tool. The performance of our technologies continues to be assessed according to the best-in-class criteria established in the V3 framework.
Verification
The GENEActiv records unfiltered, sensor-level acceleration as well as light and temperature in SI units. The engineering validation is supported by internal infrastructure, processes and documentation managed under ISO13485 and ISO27001. The quality of the raw data collected underpins all our work and is recognised by external verification of measurement consistency (Esliger 2011, Ladha 2013), acceleration processing (van Hees 2013), sleep measurement (te Lindert 2013), sleep cycle determination (van Hees 2015) and assessment of activities of daily living (Rowlands 2014, Burton 2018).
Helpful Resources
Let us help guide you along your Sleep Digital Measure journey. Below are some useful resources:
- Our Digital Measures Catalogue
- GENEActiv; wearable used in 60 + sleep publications and clinical trials
- DATAcc by DiMe, Core Digital Measures of Sleep
- The V3 Framework – DATAcc by DiMe (dimesociety.org)
References
- Jääkallio, P., Kuula, L., & Pesonen, A.-K. (2024). Temporal pathways between circadian rhythm, depression, and anxiety in the transition from adolescence to early adulthood. Journal of Affective Disorders, 350, 656-664. DOI: 10.1016/j.jad.2024.01.023
- Jenkins, C. A., Tiley, L. C. F., Lay, I., Hartmann, J. A., Chan, J. K. M., & Nicholas, C. L. (2022). Comparing GENEActiv against Actiwatch-2 over Seven Nights Using a Common Sleep Scoring Algorithm and Device-Specific Wake Thresholds. Behavioral Sleep Medicine, 20(4), 369-379. DOI 10.1080/15402002.2021.1924175
- Sim, J. E., Leota, J., Mascaro, L., Hoffman, D., & Facer-Childs, E. R. (2024). Sleep patterns before and after competition: A real-world examination of elite athletes. Journal of Sports Sciences, 42(12), 2014-2026. DOI: 10.1080/02640414.2024.2308960
- te Lindert, B. H. W., & Van Someren, E. J. W. (2013). Sleep estimates using microelectromechanical systems (MEMS). Sleep, 36(5), 781-9. DOI:10.5665/sleep.2648
- Lindert BHW, Blanken TF, van der Meijden WP, et al. Actigraphic multi‐night home‐recorded sleep estimates reveal three types of sleep misperception in Insomnia Disorder and good sleepers. J Sleep Res. 2020;29: e12937. DOI: https://doi.org/10.1111/jsr.12937
- Antczak, D., Lonsdale, C., del Pozo Cruz, B., Parker, P., & Sanders, T. (2021). Reliability of GENEActiv accelerometers to estimate sleep, physical activity, and sedentary time in children. International Journal of Behavioral Nutrition and Physical Activity, 18, Article 73. DOI: https://doi.org/10.1186/s12966-021-01141-2
- Plekhanova, T., Rowlands, A. V., Evans, R. A., Edwardson, C. L., Bishop, N. C., Bolton, C. E., … & Lone, N. I. (2022). Device-assessed sleep and physical activity in individuals recovering from a hospital admission for COVID-19: a multicentre study. International Journal of Behavioral Nutrition and Physical Activity, 19, Article 94. DOI: https://doi.org/10.1186/s12966-022-01333-w
- Vázquez-Sánchez, María Ángeles; Corral Pérez, Juan; Naranjo Marquez, María; Ponce González, Jesús Gustavo; Casals, Cristina. (2022). Relationship of accelerometer-measured inactivity and sleep efficiency with body mass index in prefrail elders. https://hdl.handle.net/10630/25168
- De Looze, C., Scarlett, S., Newman, L., & Kenny, R. A. (2022). Sleep duration and disturbance are associated with orthostatic heart rate recovery: Findings from the Irish Longitudinal Study on Ageing. Sleep Health: Journal of the National Sleep Foundation, 8(6), 654-662. DOI: https://doi.org/10.1016/j.sleh.2022.08.002
- Glaus, J., Kang, S. J., Guo, W., Lamers, F., Strippoli, M.-P. F., Leroux, A., Dey, D., Plessen, K. J., Vaucher, J., Vollenweider, P., Zipunnikov, V., Merikangas, K. R., & Preisig, M. (2023). Objectively assessed sleep and physical activity in depression subtypes and its mediating role in their association with cardiovascular risk factors1. Journal of Psychiatric Research, 163, 325-336. DOI: https://doi.org/10.1016/j.jpsychires.2023.05.042
- Jackson, C., Stewart, I. D., Plekhanova, T., Cunningham, P. S., Hazel, A. L., Al-Sheklly, B., … & Zongo, O. (2023). Effects of sleep disturbance on dyspnoea and impaired lung function following hospital admission due to COVID-19 in the UK: A prospective multicentre cohort study. The Lancet Respiratory Medicine, 11(8), 673-684. DOI: https://doi.org/10.1016/S2213-2600(23)00124-8
- Edgley, K., Chun, H.-Y. Y., Whiteley, W. N., & Tsanas, A. (2023). New insights into stroke from continuous passively collected temperature and sleep data using wrist-worn wearables. Sensors, 23(3), 1069. DOI: https://doi.org/10.3390/s23031069
- Kuang, B., Aarab, G., Wei, Y., Blanken, T. F., Lobbezoo, F., Van Someren, E. J. W., Ramautar, J. R., & Wassing, R. (2023). Associations between signs of sleep bruxism and insomnia: A polysomnographic study. Journal of Sleep Research, 32(4), e13827. DOI: https://doi.org/10.1111/jsr.13827cas
- van Hees, V. T., Sabia, S., Anderson, K. N., Denton, S. J., Oliver, J., Catt, M., … & others. (2015). A Novel, Open Access Method to Assess Sleep Duration Using a Wrist-Worn Accelerometer. PLoS ONE, 10(11), e0142533. DOI: https://doi.org/10.1371/journal.pone.0142533
- Nascimento-Ferreira, M. V., Collese, T. S., de Moraes, A. C. F., Rendo-Urteaga, T., Moreno, L. A., & Carvalho, H. B. (2016). Validity and reliability of sleep time questionnaires in children and adolescents: A systematic review and meta-analysis12. Sleep Medicine Reviews, 30, 85-96. DOI: https://doi.org/10.1016/j.smrv.2015.11.006
- O’Donnell, J., Hollowell, S., Salimi-Khorshidi, G., Velardo, C., Sexton, C., Rahimi, K., Johansen-Berg, H., Tarassenko, L., & Doherty, A. (2017). Automated detection of sleep-boundary times using wrist-worn accelerometry. BioRxiv. DOI: https://doi.org/10.1101/225516
- Sansom, K., Reynolds, A., McVeigh, J., Mazzotti, D. R., Dhaliwal, S. S., Maddison, K., Walsh, J., Singh, B., Eastwood, P., & McArdle, N. (2023). Estimating sleep duration: Performance of open-source processing of actigraphy compared to in-laboratory polysomnography in the community. SLEEP Advances, 4(1). DOI: https://doi.org/10.1093/sleepadvances/zpad028
- Zijlmans, J. L., Riemens, M. S., Vernooij, M. W., Ikram, M. A., & Luik, A. I. (2023). Sleep, 24-Hour Activity Rhythms, and Cognitive Reserve: A Population-Based Study1. Journal of Alzheimer’s Disease, 91(2), 663-672. DOI: https://doi.org/10.3233/JAD-220714
- Burton, E., Hill, K. D., Lautenschlager, N. T., Thøgersen-Ntoumani, C., Lewin, G., Boyle, E., & Howie, E. (2018). Reliability and validity of two fitness tracker devices in the laboratory and home environment for older community-dwelling people1. BMC Geriatrics, 18(103). DOI: https://doi.org/10.1186/s12877-018-0792-4
- Cassidy, S., Trenell, M., Stefanetti, R. J., Charman, S. J., Barnes, A. C., Brosnahan, N., McCombie, L., Thom, G., Peters, C., Zhyzhneuskaya, S., Leslie, W. S., Catt, C., Catt, M., McConnachie, A., Sattar, N., Sniehotta, F. F., Lean, M. E.J., & Taylor, R. (2023). Physical activity, inactivity and sleep during the Diabetes Remission Clinical Trial (DiRECT). Diabetic Medicine, 40(3), e15010. DOI: 10.1111/dme.15010
- Papandreou, C., Díaz-López, A., Babio, N., Martínez-González, M. A., Bulló, M., Corella, D., Fitó, M., Romaguera, D., Vioque, J., Alonso-Gómez, Á. M., Wärnberg, J., Martínez, A. J., Serra-Majem, L., Estruch, R., Fernández-García, J. C., Lapetra, J., Pintó, X., Tur, J. A., Garcia-Rios, A., & Bueno-Cavanillas, A. (2019). Long Daytime Napping Is Associated with Increased Adiposity and Type 2 Diabetes in an Elderly Population with Metabolic Syndrome. Journal of Clinical Medicine, 8(7). DOI: 10.3390/jcm8071053
- Devenney, L. E., Coyle, K. B., Roth, T., & Verster, J. C. (2019). Sleep after Heavy Alcohol Consumption and Physical Activity Levels during Alcohol Hangover. Journal of Clinical Medicine, 8(5), 752. DOI: 10.3390/jcm8050752
- Casals C, Ávila-Cabeza-de-Vaca L, González-Mariscal A, Marín-Galindo A, Costilla M, Ponce-Gonzalez J G, Vázquez-Sánchez M Á, Corral-Pérez J (2023) Effects of an educational intervention on frailty status, physical function, physical activity, sleep patterns, and nutritional status of older adults with frailty or pre-frailty: the FRAGSALUD study. Frontiers in Public Health. 11(1267666). DOI: 10.3389/fpubh.2023.1267666
- Cheong, S.-M., & Gaynanova, I. (2024). Sensing the impact of extreme heat on physical activity and sleep. Digital Health, 20552076241241509. DOI: https://doi.org/10.1177/20552076241241509
- Kolk, M. Z. H., Frodi, D. M., Langford, J., Meskers, C. J., Andersen, T. O., Jacobsen, P. K., Risum, N., Tan, H. L., Svendsen, J. H., & Knops, R. E. (2023). Behavioural digital biomarkers enable real-time monitoring of patient-reported outcomes: A substudy of the multicenter, prospective observational SafeHeart study. European Heart Journal – Quality of Care and Clinical Outcomes. Advance online publication. DOI: 10.1093/ehjqcco/qcad069
- Rosique-Esteban, N., Papandreou, C., Romaguera, D., Warnberg, J., Corella, D., Martínez-González, M. Á., Díaz-López, A., Estruch, R., Vioque, J., & Arós, F. (2018). Cross-sectional associations of objectively measured sleep characteristics with obesity and type 2 diabetes in the PREDIMED-Plus trial. Sleep, 41(12). DOI: 10.1093/sleep/zsy190
- Rowlands, A. V., Olds, T. S., Hillsdon, M., Pulsford, R., Hurst, T. L., Eston, R. G., Gomersall, S. R., Johnston, K., & Langford, J. (2014). Assessing sedentary behavior with the GENEActiv: introducing the sedentary sphere. Medicine & Science in Sports & Exercise, 46(6). DOI: 1235-1247.
- Esliger, D. W., Rowlands, A. V., Hurst, T. L., Catt, M., Murray, P., & Eston, R. G. (2011). Validation of the GENEA Accelerometer. Medicine & Science in Sports & Exercise, 43(6). DOI: 1085-1093.
- Ladha, C., Jackson, D., Ladha, K., Nappey, T., & Olivier, P. (2013). Shaker table validation of OpenMovement accelerometer. Ambul Monit Phys Act MovAt: Amherst MA. DOI: 10.13140/RG.2.2.31312.51208.
- van Hees, V. T., Gorzelniak, L., Dean León, E. C., Eder, M., Pias, M., Taherian, S., … Brage, S. (2013). Separating Movement and Gravity Components in an Acceleration Signal and Implications for the Assessment of Human Daily Physical Activity. PLoS ONE, 8(4), e61691. DOI: 10.1371/journal.pone.0061691


